Cardiovascular disorders after the third dose of COVID-19 vaccine
Most cases of cardiovascular adverse events in vaccine recipients occur following the second dose. Cases following the third dose of COVID-19 vaccines have been also reported. The risk was about the same as after the 2nd dose. We discussed a fatal case of a 26-year-old male who did not have any side effects from his two previous doses. Here are two similar cases with subsequent resolution.
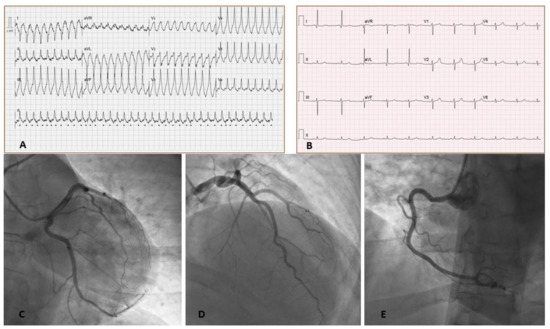
A 43-year-old female with no past medical history presented with palpitations and shortness of breath started 2 days after receiving the third dose of BNT162b2 COVID-19 vaccine. No side effects of the vaccine were noted following the preceding two doses received five months prior. On presentation, her electrocardiogram showed rapid monomorphic ventricular tachycardia (VT) requiring a synchronized cardioversion (see Figure).
Laboratory blood tests showed normal complete blood count, elevated C-reactive protein up to 6.7 mg/dl, and high-sensitive troponin I up to 2082 ng/L. D-dimer was also elevated at 1.3 ng/L, but a Chest CT angiography ruled out acute pulmonary embolism. Polymerase-chain-reaction (PCR) tests of nasopharyngeal swab obtained on admission for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and for other viruses causing upper respiratory tract infection was negative.
The patient was treated with prednisone (1 mg/kg, with gradual dose tapering over the next 3 months), bisoprolol, and ramipril, with complete resolution of symptoms, inflammatory markers, and troponin elevation. Her LV systolic function remained mildly to moderately reduced, and given her presentation with life-threatening arrhythmia, the patient was discharged home with a wearable defibrillator (LifeVest) while on steroid therapy.
A 62-year-old woman diagnosed in September 2019 of lung adenocarcinoma stage IV, carrier of an EGFR mutation (Ex19Del) on treatment with osimertinib, developed fever and hypotension 24 h after administration of the third dose of Moderna® COVID-19 vaccine in the context of acute myocarditis with evidence of severe left ventricular (LV) dysfunction.
Cardiac magnetic resonance imaging (MRI) showed evidence of global myocardial oedema compatible with acute myocarditis. Coronary CT showed a lesion in the anterior descending coronary artery requiring revascularization. A few days later, she presented febrile symptoms with isolation of Staphylococcus aureus in the central line catheter and antibiotherapy with cloxacillin was started, with subsequent resolution of the infectious symptoms.
A 73 years-old woman presented with shortness of breath and fatigue 2 weeks after receiving her second dose of BNT162b2 SARS-CoV-2 mRNA vaccine. ECG showed complete AV block with normal narrow QRS complexes. Chronic treatment with Bisoprolol for hypertension was stopped but complete AV block persisted 48 hours thereafter. Therefore, a permanent pacemaker was implanted. Three months later, pacemaker follow-up revealed no ventricular stimulation, suggesting complete recovery of AV conduction, even after resumption of bisoprolol. Five months after the second dose, she received a third dose of the same vaccine. Three weeks later, she once again complained of dyspnea on exertion. ECG showed sinus rhythm but complete AV block persisted 48 hours thereafter. Therefore, a permanent pacemaker was implanted. Three months later, pacemaker follow-up revealed no ventricular stimulation, suggesting complete recovery of AV conduction, even after resumption of bisoprolol. Five months after the second dose, she received a third dose of the same vaccine. Three weeks later, she once again complained of dyspnea on exertion. ECG showed sinus rhythm with permanent ventricular stimulation. After device inhibition, complete AV block was confirmed and, 2 weeks later, conduction was restored once more.
REFERENCES
Mengesha B, Asenov AG, Hirsh-Raccah B, Amir O, Pappo O, Asleh R. Severe acute myocarditis after the third (booster) dose of mRNA COVID-19 vaccination. Vaccines. 2022 Apr 8;10(4):575.
Etienne H, Charles P, Pierre T. Transient but recurrent complete heart block in a patient after COVID-19 vaccination–A case report. Annals of Medicine and Surgery. 2022 Jun 1;78:103694.
Brage ET, Ruíz JR, Martín JG, Rodríguez JD, Tocino RV, Diego SR, Hernández PL, Hernández LB, Sánchez EF. Fulminant myocarditis in a patient with a lung adenocarcinoma after the third dose of modern COVID-19 vaccine. A case report and literature review. Current Problems in Cancer: Case Reports. 2022 Jun 1;6:100153.



Comments
Post a Comment