Analysis of antiviral T cell responses by IFN-γ ELISPOT showed that Spike-specific T cell activation was induced by vaccination and infection, as expected after receiving Spike protein-based vaccines. The patient’s non-Spike responses (to Nucleocapsid) were enhanced as well after receiving the Moderna vaccine booster dose. Nirmatrelvir/ritonavir treatment resulted in the retention of Spike- but not Nucleocapsid-specific T cell responses, while halting tocilizumab correlated with elevated T cell responses against both proteins. Resumption of tocilizumab subsequently decreased T cell responses to both viral antigens.
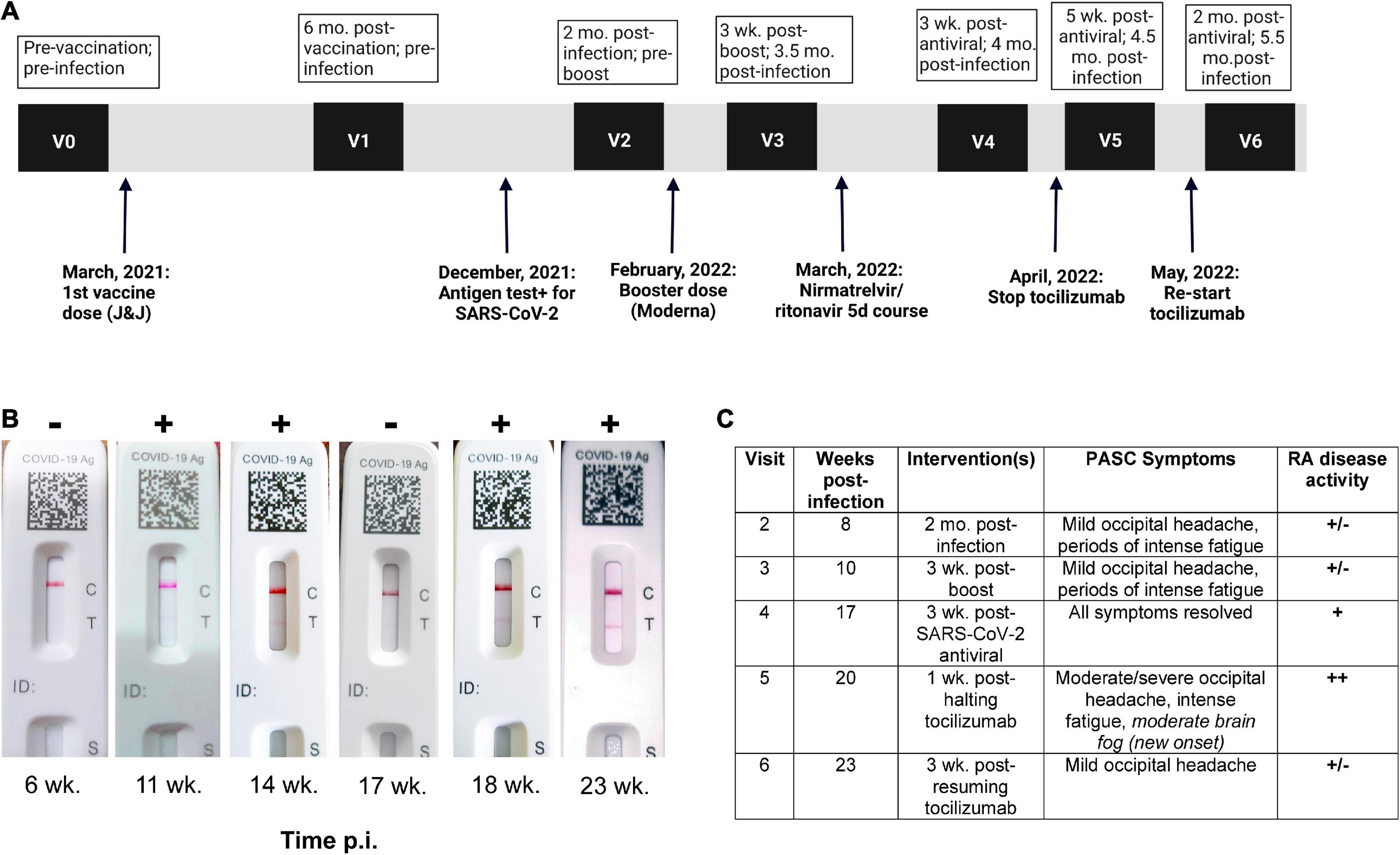
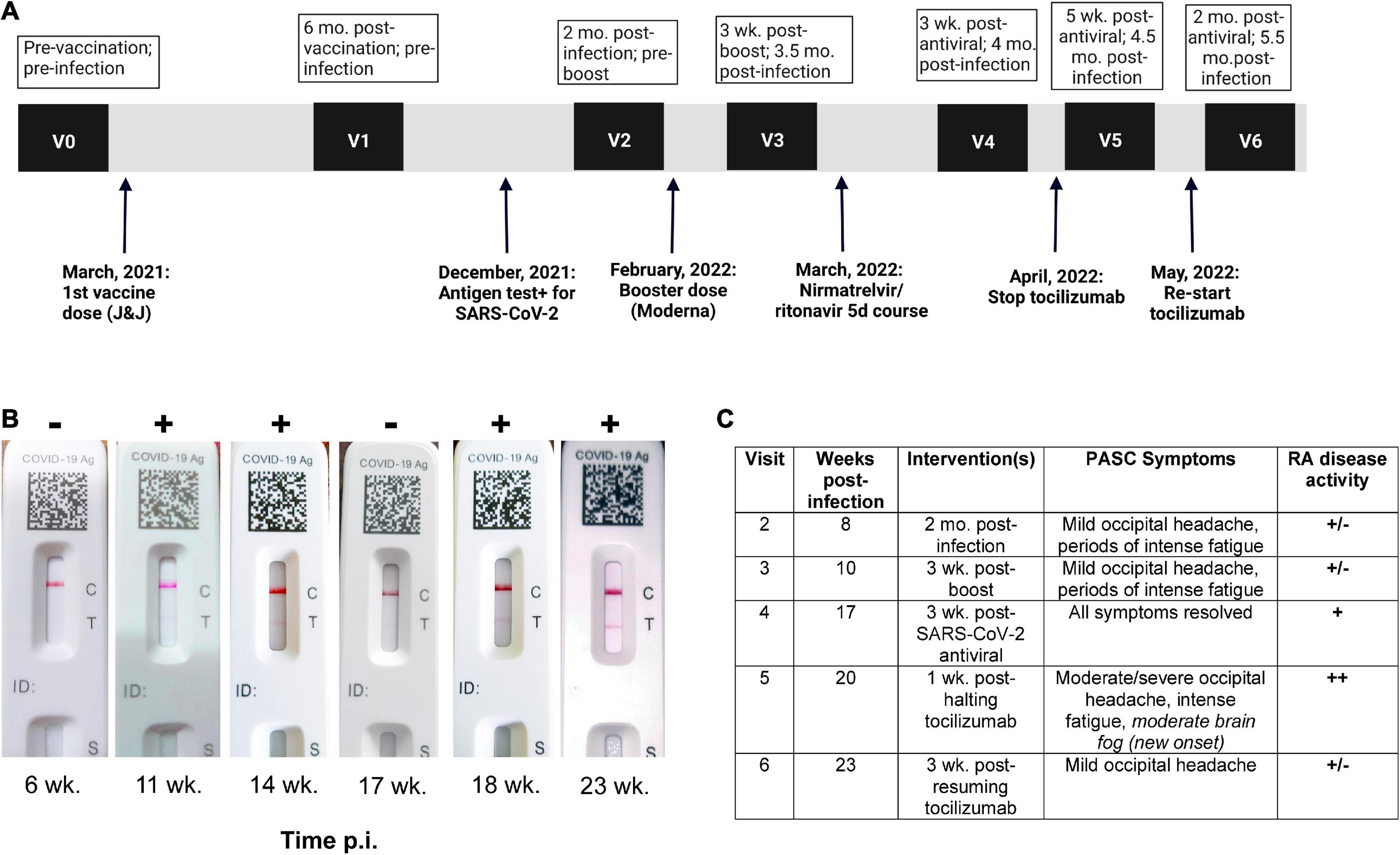
The patient’s mild acute symptoms combined with an escalation in Neuro-PASC symptom severity after stopping tocilizumab, as well as their resolution after resuming treatment suggests that IL-6 blockade should be studied further as a potential therapeutic intervention for Neuro-PASC.
REFERENCE
Visvabharathy L, Orban ZS, Koralnik I. Case Report: Treatment of long COVID with a SARS-CoV-2 antiviral and IL-6 blockade in a patient with rheumatoid arthritis and SARS-CoV-2 antigen persistence. Frontiers in Medicine.:2832.



Comments
Post a Comment