Rapidly Progressive Dementia Following COVID-19 Vaccination
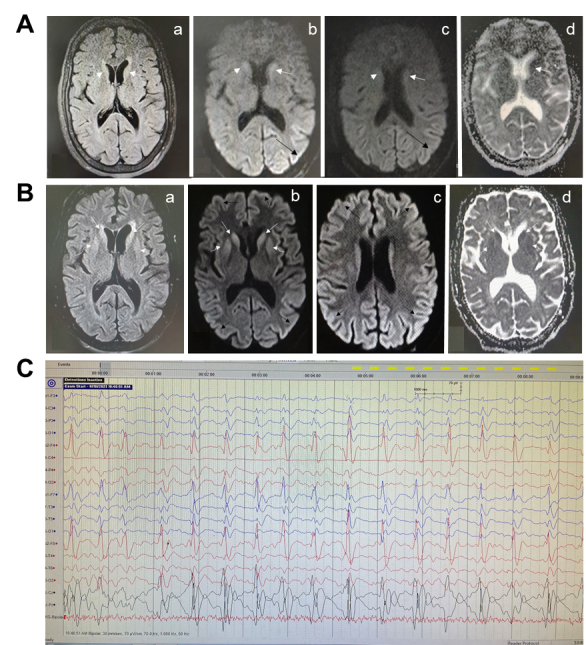
A previously healthy woman in her 60s had mild fever and uneventful course after the 1st dose of ChAdOx1 nCoV-19 vaccine, but developed behavioral problems and refusal to take food, one day after receiving the second dose of ChAdOx1 nCoV-19 vaccination (dose interval 84 days). Her condition progressed rapidly with onset of confusion, forgetfulness, and hallucinations within the next 5 days. Over the next two days, the patient developed difficulty in walking and echolalia. She was prescribed amantadine, trihexyphenidyl and clonazepam by a local practitioner but she showed further deterioration in the form of irritability, incoherent speech, aggravated forgetfulness, auditory and visual hallucinations, abnormal movements of limbs, and jaw and neck dystonia. The patient had a serum anti-Spike protein IgG titer of 1891.5 AU/mL (non-reactive<50 AU/mL) at 37 days post-second dose. An initial magnetic resonance imaging (MRI) of the brain had revealed FLAIR hyperintensity in bilateral caudate heads which showed diffusion restriction and also patchy diffusion restriction in the left posterior parietal and occipital gyri (Fig. 1A).
In the absence of clinical improvement, a repeat imaging was performed after 16 days (Fig. 1B) which revealed an increase in the degree of FLAIR hyperintensity and diffusion restriction in bilateral caudate nuclei as well as involvement of bilateral putamina, with diffuse diffusion restriction in the cerebral cortex in bilateral hemispheres. A cortical ribboning pattern of hyperintensity was observed in the diffusion image.
An electroencephalogram (EEG) revealed bilateral biphasic and triphasic sharp wave periodic discharges of around one Hz, with slowing of background activity (Fig. 1C). The patient was managed conservatively with a trial of dexamethasone, empirical broad-spectrum antibiotics, and antiepileptics but had no significant improvement. Later, bromocriptine was added which resulted in some improvement in her limb rigidity. However, overall neurologic deterioration continued over the next two weeks, and she developed respiratory distress and shock to which she finally succumbed after one month of admission. The possibility of a secondary infection leading to sepsis and shock, and eventually resulting in fatality exists.
Another case of a 30-year-old woman presented with rapidly progressive dementia 1 month after COVID-19
People with dementia differ biologically from cognitively healthy older adults in several relevant ways: * **Chronic neuroinflammation** and microvascular damage * **Immunosenescence** (aging immune system) * **Reduced physiological reserve** (less ability to compensate for stress) * Higher burden of **comorbidities** (diabetes, atherosclerosis, stroke history) Because of this, *any systemic stressor* (infection, dehydration, surgery, medication change) can cause: * Delirium * Stepwise cognitive decline * Functional deteriorationREFERENCE
Chakrabarti SS, Tiwari A, Jaiswal S, Kaur U, Kumar I, Mittal A, Singh A, Jin K, Chakrabarti S. Rapidly Progressive Dementia with Asymmetric Rigidity Following ChAdOx1 nCoV-19 Vaccination. Aging Dis. 2022 Jun 1;13(3):633-636. doi: 10.14336/AD.2021.1102. PMID: 35656106; PMCID: PMC9116920.



Comments
Post a Comment