HLA-A*11 and vaccine-induced thyroiditis
The human leukocyte antigen (HLA) genes encode proteins essential for mounting an immune response. Immune systems of people with specific HLA types may be better or worse at mounting an immune response and generating antibodies to specific proteins.
HLA-A11 (A11) is one of serotypes with 10.8% frequency in worldwide population. It's most common in East Asia. One of its variations, HLA-A*11, has been linked with vaccine-induced subacute thyroiditis (V-SAT). This rare transient inflammatory thyroid disease is usually associated with pain and tenderness of the gland, as well as generalized somatic symptoms: from anxieties, difficulty swallowing, changes in appetite, malaise and fatigue to complete prostration for weeks or months if left untreated. HLA-A*11:01:01:01 was found to be significantly associated with the severity of COVID-19.
SAT is the most common thyroid dysfunction following SARS-CoV-2 vaccination. There have been multiple reports of post-vaccination thyrotoxicosis, including in genetically tested individuals.
A healthy 48-year-old male with a three-week history of right neck swelling, throat discomfort, palpitations, fevers, and weight loss of 10 pounds - started one week after administration of the second dose of the SARS-CoV-2 vaccine, was diagnosed with V-SAT in Boston, MA. Laboratory testing was notable for an elevated C-reactive protein (CRP) hyperthyroidism (free T4 level of 3.6 ng/dL, thyroid-stimulating hormone (TSH) level of 0.01 uIU/mL). He had an excellent clinical response to initiation of NSAIDs and glucocorticoid therapy with rapid symptomatic improvement after the first dose of prednisone.
A middle-aged woman presented with painful thyroid swelling following the second dose of the COVID-19 mRNA vaccine BNT162b2 (Pfizer-BioNTech) with clinical, biochemical and imaging features consistent with destructive thyrotoxicosis. She had 36 hrs of flu-like symptoms following vaccination. Two weeks later she noticed that her neck was painful. She lost 10 pounds suffering from appetite loss, sweating and frequent trips to bathroom. Her mother had thyroid cancer when she was young and mother's sister and her sister’s son have Hashimoto’s thyroiditis. The patient was managed conservatively with a course of Non-steroidal anti-inflammatory drugs (NSAIDs) for her pain relief. As her thyrotoxicosis symptoms rapidly resolved, she did not require any antithyroid medication or beta-blocker. At her follow up review at 3 months, she continued to remain clinically and biochemically euthyroid.
A 42yo female with no past medical history received the first dose of the Pfizer/BioNTech mRNA vaccine for COVID-19. Five days later, the patient complained of sore throat and palpitations. These symptoms progressed and she was evaluated in an urgent care one week after vaccination where she was found to have tachycardia. Infectious work-up, including PCR for COVID-19, was negative and she was sent home. She took ibuprofen with some improvement of her symptoms. The following day she went to the ED; she was found to have a heart rate in the 130s with sinus tachycardia on EKG. Thyroid function testing was done which revealed TSH <0.01, fT4 4.58, fT3 11.8. Her TPO antibody was <28 and inflammatory markers were elevated including sed rate of 62. The patient was prescribed prednisone 40mg daily and propranolol 20mg and reported rapid improvement of symptoms with prednisolone.
A case of subacute thyroiditis 3 days after receiving the second dose of inactivated SARS-CoV-2 vaccine (BBIBP-CorV) was documented for a 32-year-old female. Her symptoms started 3 days after the second dose.
A 29-year-old previously healthy Sri-Lankan woman complained of anterior neck pain, low-grade fever and fatigue appearing 7days after immunization with the second dose of inactivated SARS-CoV-2 – Sinopharm vaccine. The patient was treated symptomatically with non-steroidal anti-inflammatory drugs (NSAIDs). Her neck pain and tenderness resolved gradually.
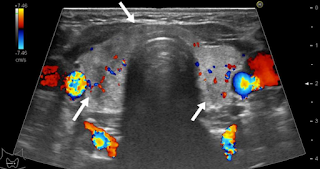
Three female healthcare workers were diagnosed with V-SAT after inactivated Coronavac vaccine. The figure shows bilateral hypoechoic areas with irregular borders and reduced blood flow in Doppler USG for one of them with a mild case.
Two Polish males (61- and 45- year old) diagnosed with V_SAT both had HLA-B*35:03 and -C*04:01 allelesco-present with HLA-A*03:01, -DQA1:01, and DQB1*05:01.
When the HLA phenotypes of the patient group (V-SAT and non-V-SAT groups both) and the control group were compared, it was found that positivity rates for HLA-A*11, HLA-B*35, and HLA-C*04 alleles were higher in the patient group. These alleles were found to be related to increased risk with odds ratios of 2.8, 23.7, and 10.9, respectively. There was no homozygosity for these alleles at any of the patient group’s HLA-A, B, and C loci. The HLA-B*35 allele was present in 92.6% (25/27) of the patient group and 34.5% (125/362) of the control group.
REFERENCES
Stasiak M, Zawadzka-Starczewska K, Lewiński A. Significance of HLA Haplotypes in Two Patients with Subacute Thyroiditis Triggered by mRNA-Based COVID-19 Vaccine. Vaccines. 2022 Feb 11;10(2):280.
Şendur SN, Özmen F, Oğuz SH, İremli BG, Malkan ÜY, Gürlek A, Erbas T, Ünlütürk U. Association of Human Leukocyte Antigen Genotypes with Severe Acute Respiratory Syndrome Coronavirus 2 Vaccine-Induced Subacute Thyroiditis. Thyroid. 2022 May 9.
Sahin Tekin M, Yorulmaz G, Yantir E, Gunduz E, Colak E. A Novel Finding of an HLA Allele’s and a Haplotype’s Relationship with SARS-CoV-2 Vaccine-Associated Subacute Thyroiditis. Vaccines. 2022 Dec;10(12):1986.
Jeeyavudeen MS, Patrick AW, Gibb FW, Dover AR. COVID-19 vaccine-associated subacute thyroiditis: an unusual suspect for de Quervain's thyroiditis. BMJ Case Rep. 2021 Nov 9;14(11):e246425. doi: 10.1136/bcr-2021-246425. PMID: 34753732; PMCID: PMC8578953.
Patel KR, Cunnane ME, Deschler DG. SARS-CoV-2 vaccine-induced subacute thyroiditis. American Journal of Otolaryngology. 2022 Jan;43(1):103211.
Franquemont S, Galvez J. Subacute Thyroiditis After mRNA Vaccine for Covid-19. J Endocr Soc. 2021 May 3;5(Suppl 1):A956–7. doi: 10.1210/jendso/bvab048.1954. PMCID: PMC8089609.
Yorulmaz G, Sahin Tekin M. SARS-CoV-2 vaccine-associated subacute thyroiditis. Journal of Endocrinological Investigation. 2022 Feb 19:1-7.
Pi L, Lin J, Zheng Y, Wang Z, Zhou Z. Case report: subacute thyroiditis after receiving inactivated SARS-CoV-2 vaccine (BBIBP-CorV). Frontiers in medicine. 2022;9.
Wijenayake UN, Ratnayake GM, Abeyratne D, Bulugahapitiya US. A case report of subacute thyroiditis after inactivated SARS-CoV-2 vaccine. SAGE Open Medical Case Reports. 2022 Nov;10:2050313X221140243.



Comments
Post a Comment