Multisystem Inflammatory Syndrome in Children after SARS-CoV-2 Vaccination
Multisystem inflammatory syndrome in children (MIS-C) and adults (MIS-A) can follow SARS-CoV-2 infection. MIS-C was primarily described for 16-20 year olds, racial/ethnic minority populations and children with comorbidities.
MIS-C and MIS-A can be also induced by vaccination without current COVID-19 infection. In adults, many individuals who experienced it were vaccinated 11-78 days after COVID-19-like illness. One case when a 30-year-old male was vaccinated 6 and 28 days after positive test was fatal. In children, only ~25% had COVID-19 in the past. Average age was lower than in MIS-C triggered by the virus.
Here are a few case reports.
A previously healthy 12-year-old male presented with a 4-day duration of fever, eye redness, diarrhea, neck pain and swelling that started 27 days before his first dose of Pfizer-BioNTech COVID-19 vaccine.
He had no history of COVID-19 infection or exposure. He had a negative anti-SARS-CoV-2 nucleocapsid total antibody level, but a high level of anti-SARS-CoV-2 spike IgG (257 BAU/mL; >0.8 BAU/mL: positive result), indicating a vaccine-induced antibody response rather than a SARS-CoV-2 infection-induced antibody response. He was treated with IVIG (2 g/kg) and methylprednisolone (2 mg/kg). He was discharged 5 days after admission with no sequela or complication.
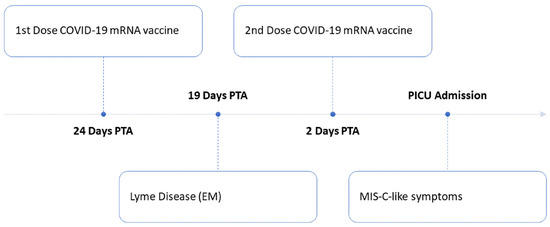
(Fig.1).
A 12-year-old boy presented by continuous, high-grade fever for 3 days, redness of eyes, followed by a diffuse erythematous non-itchy rash, fatigue and abdominal pain, 5 weeks after his second dose of Moderna vaccine that was preceded by the first dose of Pfizer-BioNTech vaccine given 3 weeks apart. He had no history of COVID-19 infection or exposure. He was treated with intravenous fluids, acetaminophen, antibiotics and intravenous immunoglobulin. One week after discharge he only had residual mild fatigue.
A 15-year-old boy with a history of mild COVID-19 received the first dose of COVID-19 messenger RNA vaccine (Moderna) 50 days later. On post-vaccination day 1, the patient developed fever, lethargy, headache, diarrhea, nausea, lip swelling, and right neck pain. On post-vaccination day 4, he sought medical consultation because his condition worsened. Intravenous immunoglobulin (IVIG) was initiated at 1 g/kg/day, and oral aspirin was started at 200 mg (3 mg/kg/day). The patient subsequently recovered without relapse.
A 15-year-old girl with asthma received her first dose of BNT162b2 6 days before seeking care. She had low-grade fever and myalgia, which resolved within 2 days of vaccination. Four days later, she experienced 102°F fevers, headaches, nonbilious emesis, bilateral conjunctivitis, myalgias, chest pain, pharyngeal erythema and a diffuse blanching rash. She was negative for SARS-CoV-2. She was admitted to the pediatric intensive care unit (ICU) and given 2 g/kg intravenous immune globulin (IVIG) for suspected of Multisystem Inflammatory Syndrome in Children MIS-C. The patient fully recovered.
A previously healthy female 17-year-old received her first dose of BNT162b2 vaccination 7 days before seeking care. Three days after vaccination, she experienced fevers, headaches, abdominal pain, fatigue, and myalgias. Laboratory test results showed leukocytosis with polymorphonuclear cell predominance and elevated CRP, erythrocyte sedimentation rate, lactate dehydrogenase, BNP, troponin, D-dimer, creatinine, aspartate aminotransferase, and alkaline phosphate. Urine culture was positive for 10,000 CFU/mL of Escherichia coli. Electrocardiogram showed sinus tachycardia and nonspecific T-wave abnormalities. SARS-CoV-2 RT-PCR was negative, but spike antibody testing was positive. She was treated with methylprednisolone and IVIG, and for a possible UTI. She was discharged on hospital day 4 with down-trending inflammatory markers.
A healthy 14-year-old boy experienced 3 days of coughing and congestion and tested positive by PCR for SARS-CoV-2 infection one month after completing the Pfizer-BioNTech 2-dose COVID-19 vaccine series (Figure). He recovered from COVID-19 but developed Multisystem Inflammatory Syndrome with pericardial effusion.
An otherwise healthy 14-year-old girl was diagnosed with COVID-19 three months after completing the 2-dose Pfizer-BioNTech COVID-19 vaccine series (Figure). At readmission on day 19, differential diagnoses included MIS-C, acute COVID-19 with hyperinflammation, sepsis, toxic shock syndrome, drug reaction, and vasculitis or other autoimmune disease. Echocardiogram results were unremarkable.
These findings indicate that even full COVID-19 vaccination in adolescents is not 100% effective against MIS-C.
REFERENCES
Abdelgalil AA, Saeedi FA. Multisystem inflammatory syndrome in a 12-year-old boy after mRNA-SARS-CoV-2 vaccination. The Pediatric infectious disease journal. 2022 Mar;41(3):e93.
Poussaint TY, LaRovere KL, Newburger JW, Chou J, Nigrovic LE, Novak T, Randolph AG. Multisystem inflammatory-like syndrome in a child following COVID-19 mRNA vaccination. Vaccines. 2021 Dec 30;10(1):43.
Koga T, Yoshimura M, Kubo S, Nagai M, Tabata K, Teranishi H, Fujino M, Kawana H, Musha I, Akioka Y. Multisystem Inflammatory Syndrome after COVID-19 Vaccination (MIS-V) Presenting with Retropharyngeal Phlegmon in a 15-year-old Boy in Japan. American Journal of Medical Case Reports. 2022 Jan 23;10(2):35-8.
Jain E, Donowitz JR, Aarons E, Marshall BC, Miller MP. Multisystem inflammatory syndrome in children (MIS-C) after SARS-CoV-2 vaccination. Emerg Infect Dis. 2022 May [cited on 3/11/2022]. https://doi.org/10.3201/eid2804.212418
Cole LD, Slate M, Minneman S, Bozzella MJ. Multisystem inflammatory syndrome after breakthrough SARS-CoV-2 infection in 2 immunized adolescents, United States. Emerg Infect Dis. 2022 July. https://doi.org/10.3201/eid2807.220560




Comments
Post a Comment